Training doctors of the future

At the University of Surrey’s School of Medicine, which opened its doors in September 2024, students will undertake an intensive, four-year journey to becoming doctors of the future. But what does it take to meet the needs of a changing profession? Adapting a curriculum to embrace technology is part of the answer: from trialling the use of extended reality (XR) to teach anatomy and surgery, to giving students access to a wealth of digital resources to develop their skills, Surrey’s medical students will be prepared to excel in the world of modern medicine.
Technology-enhanced learning
Training doctors of the future, equipped with the necessary technological and digital skills, aligns with the NHS Long Term Workforce Plan to introduce innovative ways of working in the healthcare sector. Surrey’s graduate-entry course also supports the aim to grow the number of new doctors; in 2024 the government has announced that it would fund 350 places for home students at medical schools across the UK for September 2025 entry – and 34 of those places were allocated to Surrey.
Professor Juliet Wright, Founding Dean, School of Medicine, says: “We are delighted to be playing such a significant part in delivering the expansion in medical school places. New doctors qualifying from Surrey will receive training that draws on the University’s expertise in biomedical science, clinical education, technology, and digital learning.”
Professor Juliet Wright (Photo: Dean Whiting)
Professor Juliet Wright (Photo: Dean Whiting)
Surrey’s School of Health Sciences has long championed innovative, tech-enhanced training for its students: the Surrey Clinical Simulation Centre, home to two wards, a critical care unit, an ambulance bay, an immersive learning environment and a community flat, simulates real healthcare settings.
Students practise their skills on interactive manikins that move, speak and react and can be controlled by technical staff, who can alter vital signs such as breathing, pulse, blood pressure and oxygen saturation. There are manikins designed for specific clinical scenarios, such as resuscitation and birth, as well as smaller anatomic models and equipment for clinical techniques, such as cannulation and drawing blood.
All health sciences students learn the essential skills of basic life support and advanced life support in a safe environment, to ensure they have these qualifications prior to needing them on clinical placements.
The Clinical Simulation Centre also has a camera system, which uses specialist software to monitor students’ interactions in simulation classes, providing an invaluable opportunity to review footage and receive feedback; and an integrated telephone network which emulates a hospital switchboard, allowing students to practise emergency scenarios, multi-room communication and handover techniques.
Students benefit the most from this technology in the real-time simulation event that is held for all healthcare students once a year to test their skills and practise interprofessional learning. The Clinical Simulation Centre is transformed into an NHS hospital, and, with the help of actors, a range of different scenarios play out for students to react to, including mental health crises, births and accidents. Key to the success of this event is that student midwives, nurses and paramedics must work together, practising the interprofessional communication and teamwork they will experience when out in clinical practice and when beginning their careers. The event also provides a safe space in which students can practise their skills and review their performance after, with feedback from staff members. Surrey’s first cohort of medical students will participate in this event in their final year, providing a unique and highly valuable training opportunity across the two schools.
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Photo: Darren Cool
Extended reality: the future of medical training
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Professor Jag Dhanda
Prof Jag Dhanda
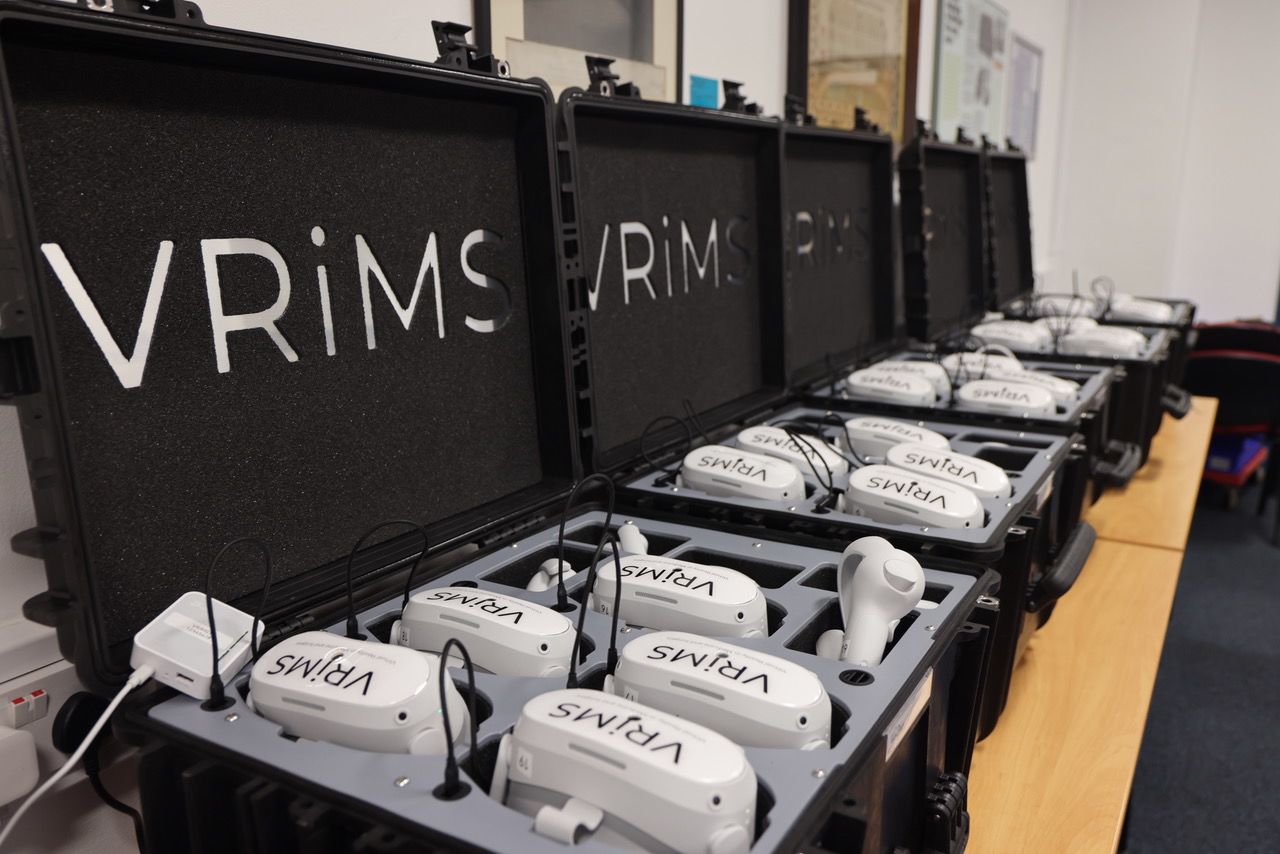
While Surrey’s aspiring doctors will benefit from the existing technology in the School of Health Sciences, their learning will go one step further. The School of Medicine has partnered with Virtual Reality in Medicine and Surgery (VRiMS), a consultancy firm that specialises in creating XR resources through virtual reality (VR), augmented reality and the metaverse with a focus on pedagogy and global health applications. First-year students will be provided with VR headsets with 3D anatomy software embedded which will be used to show different surgical techniques.
VRiMS is led by Professor Jag Dhanda, consultant oral and maxillofacial/head and neck surgeon at Queen Victoria Hospital in East Grinstead, who will be running the UK’s first fully integrated XR and hands-on surgical training courses in Surrey’s new Centre of Anatomical and Surgical Education (CASE). The training, which will be available to surgical trainees from around the UK, will use full body cadavers and will cover cardiac surgery, damage control surgery for frontline and military surgeons, transplant and organ retrieval, upper limb and hand surgery, and head and neck reconstruction surgery. Professor Dhanda will record the surgery and the footage will be used for VR training, including for Surrey’s medical students in the later years of their programme to complement their surgical placements.
Professor Dhanda says: “Current surgical training for medical students is inefficient, so providing immersive interactive experiences gives the students the best seat in the room for watching and understanding surgery. Watching a virtual reality and immersive surgical procedure maximises the experience for the student. And without it, it’s going to be very difficult to meet the government’s ambitious target of training more doctors with NHS resources that are already extremely stretched.
“The University of Surrey’s new curriculum is unique for trialling the integration of extended reality into the undergraduate training experience. And VRiMS’ application of extended reality in the training of medical students is a world-first.”
Set up during the Covid-19 pandemic as a way to deliver online training, VRiMS now has a global reach and a philanthropic outlook: to develop training resources for low- and middle-income countries (LMICs). Professor Dhanda recently returned from a trip to Africa, where he visited Ethiopia, Burundi, South Africa and Malawi, to demonstrate the VRiMS technology to LMIC surgeons, medical assistants and students who struggle to access the resources required to complete surgical training.
Professor Dhanda plans to invite African surgeons to visit CASE at Surrey over the coming years to carry out surgical procedures on cadavers. These procedures will be filmed and streamed live to colleagues in the surgeon’s home country who will view them through a VR headset. Synchronised VR training will help to create immersive surgical training resources that consider local diseases, pathology, population and resources, and demonstrate procedures in native languages.
VRiMS uses several immersive techniques, including: 360 video; 360Video with virtual studio overlay; interactive 360 video; true VR with six degrees of freedom, in which participants can move through digitally created immersive environments and manipulate digital objects; and synchronised and VR experiences. The VRiMS library of surgical videos is the world’s largest library of immersive surgical training resources, covering every surgical speciality. Medical students at Surrey will have access to this library as part of their training. If XR is fully integrated into Surrey’s Medicine curriculum in the future, students will also have access to assessment and training tools, such as fire safety training, basic life support, chest drain insertion and the ability to practise patient communications skills with virtual humans generated by artificial intelligence (AI).
Currently, creating true VR simulations with six degrees of freedom requires significant resources. Professor Dhanda explains: “Right now, it is prohibitively expensive to build even a basic simulation, but in a year or two, generative AI will change all of that, allowing simulations to be built at a fraction of the cost. I can see a time where, when undergraduate students register, they will be given a VR headset and a laptop or iPad – that is the future, and it’s coming to Surrey.”
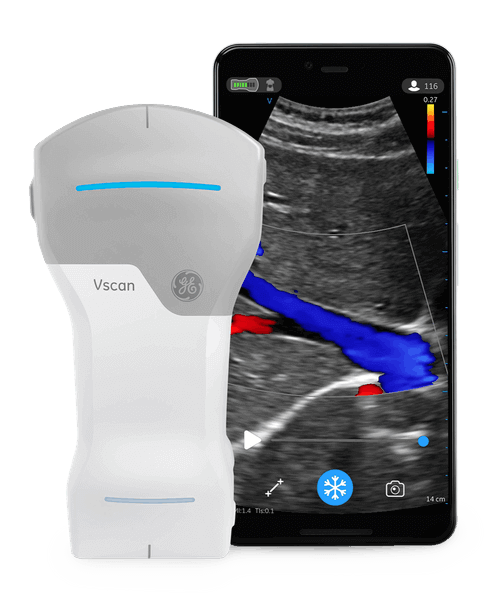
As well as using VR from the outset, Surrey’s medical students will be taught undergraduate anatomy using ultrasound scanners from Year 1. GE Vscan Air Handheld Ultrasound scanners, procured from MDI Medical, are flexible, wireless dual-probe scanners with sector and linear transducers. Students will learn the physics of how the scanners work and then learn to use them on different parts of the body.
Dr Aiden Jayanth, Head of Anatomy and Year 1 Lead, School of Medicine, says: “In the UK, anatomy is taught in a number of different ways. These range from traditional cadaver-based teaching to more modern techniques. At CASE, we will use a combination of methods, such as cadavers, extended reality, ultrasound and live streaming technology, that will complement each other. Through our collaborations with VRiMS and the Minimal Access Therapy Training Unit (MATTU), we will be at the forefront of modernising anatomy teaching whilst preserving the use of visual and tactile experiences through integrated cadaver-based teaching.”
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Photo: VRiMS
Image: MDI Medical
Image: MDI Medical
Dr Aiden Jayanth
Dr Aiden Jayanth
From physical tech to digital support
Photo: Darren Cool
Photo: Darren Cool
Dr Deborah Bruce (Photo: Darren Cool)
Dr Deborah Bruce (Photo: Darren Cool)
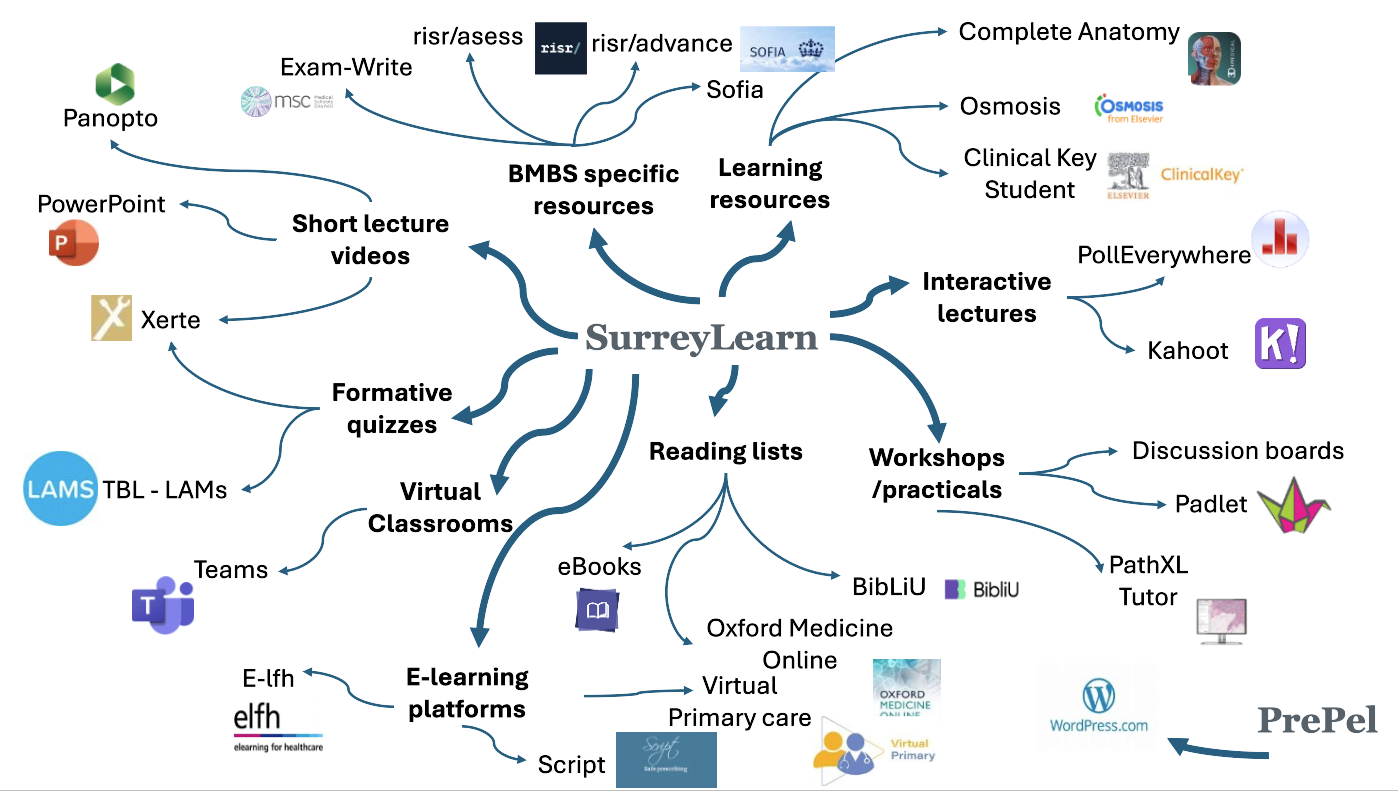
Throughout their course, Surrey’s medical students will have access to a wide range of online resources, hosted on a range of platforms including SurreyLearn, the University’s virtual learning environment. These resources include:
• an advanced 3D anatomy platform
• a curriculum mapping tool showing students what they will learn and where
• quizzes
• group learning exercises
• discussion boards.
And they can access all platforms at any time through their own University of Surrey iPad – given to every student when they start. Students will also be able to access their e-portfolio to record all their learning (both at the University and whilst on clinical placement), track their attendance, monitor their progress and develop their professional skills. This is aligned to the portfolios they will need to complete in postgraduate training.
Dr Deborah Bruce, Programme Director, School of Medicine, says: “Technology is here to stay. We must equip our future doctors with all the necessary skills to be able to work to the best of their capacity in the NHS of the future. We believe we are doing this at the University of Surrey.”
Future-ready graduates
Embracing technology is a necessary step in a rapidly changing healthcare sector, but nothing can replace genuine human interaction and hands-on learning. Surrey’s medical students will complete clinical placements with a network of partner NHS trusts throughout their four years, gaining the practical experience that is fundamental to any doctor’s training.
The School of Medicine’s objective is to equip its students with the knowledge and experience they need to excel in the world of modern medicine. Delivering a diverse, digital- and tech-enabled programme will see this commitment fulfilled, producing graduates who are ready to meet the demands of modern healthcare.
Find out more about Surrey’s Medicine course
Find out more about VRiMS and the research behind VR in medical training
Photo: Getty Images

All new medical schools must undergo an extensive period of quality assurance with the General Medical Council (GMC). Surrey’s School of Medicine has passed all stages of the accreditation process so far, with full accreditation expected when the first cohort of students graduate in 2028.